Scientists have developed a technique to rapidly and reliably detect genetic changes in Plasmodium falciparum parasites in Ghana, using just a gaming laptop and portable MinION sequencer from Oxford Nanopore Technology.
Researchers from the Wellcome Sanger Institute, University of Ghana and the Navrongo Health Research Centre were able to demonstrate for the first time that end-to-end, real-time pathogen monitoring from clinical blood samples is possible in rural, resource-limited malaria hotspots. The study looked for key drug resistance markers in the malaria parasite, and diversity in the vaccine target gene.
The findings, published in Nature Microbiology, pave the way for local monitoring of drug resistance and evaluating new malaria vaccines in affected regions themselves.
‘Powerful game changer’
Genomic surveillance – the continuous monitoring of changes in the parasite’s DNA over time – provides the tools to analyse the genomic data behind parasite drug resistance, vaccine efficacy, and evasion of rapid diagnostic tests. But until recently, it has mostly been carried out in distant labs in high-income, non-endemic countries, concentrating capacity away from affected regions.
In this new study, researchers set out to develop an accessible, near real-time method to monitor parasite mutations within the communities most affected by malaria.
This meant deploying the Oxford Nanopore MinION, a portable, pocket-sized DNA sequencer that utilises nanopore sequencing technology to analyse genetic material. This technology offers advantages such as long-read sequencing and direct detection of genetic changes.
“By taking sequencing to the source, insights arrive in days rather than years — enabling rapid, localised responses. This unprecedented speed promises to be a powerful game-changer against infectious diseases outpacing our countermeasures,” explains Edem Adika, co-first author of the study at the University of Ghana, adding the hope that this on-site approach can soon be applied to other pathogens.

Finger pricks, pocket-sized sequencers, and gaming laptops
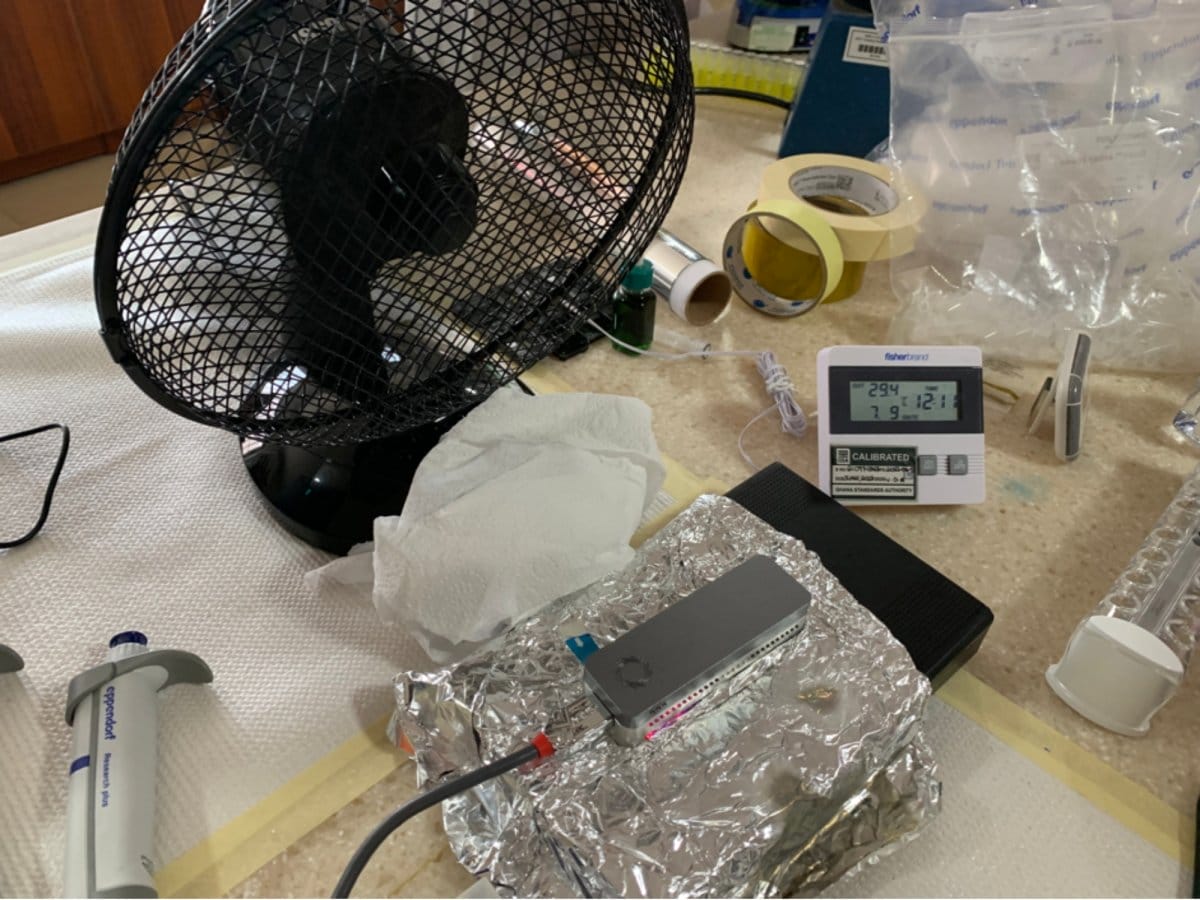
Researchers employed standard molecular biology equipment for collecting parasites from dried blood spot (DBS) samples. These are practical since they can be taken by a simple finger prick readily collected from people infected with malaria without requiring extensive resources.
They then sequenced and analysed the malaria parasite DNA using the portable MinION device and a high-specification laptop computer to detect known drug resistance markers, emerging mutations, and targets of new malaria vaccines.
The assay designed for this procedure tested parasite samples using a multiplex polymerase chain reaction (PCR), looking at five key markers in the DNA associated with changes that provided drug resistance, as well as the leading vaccine and monoclonal antibody target, circumsporozoite protein (csp). This protein helps parasites to establish infection early on after injection by feeding mosquitoes, so blocking csp helps to prevent malaria infections.
The team successfully carried out the study from two very different sites in Ghana. The first was the Ledzokuku-Krowor Municipal Assembly (LEKMA) hospital in the Ghanaian capital Accra, with its own dedicated malaria laboratory. The other part of the study took place across several community health centres in Navrongo, a rural town around 18-hours drive to the north.
They were able to generate sequencing information in as little as 48 hours after receiving a sample. Costs were kept minimal, at around £27 per sample in batches of 96.
“Sequencing P. falciparum from patients with malaria and genotyping variants that cause drug resistance – within two days of collecting the samples – felt like being in a sci-fi movie,” says Felix Nenyewodey, based at the Navrongo Health Research Centre. “This portable device (the MinION) opened our minds to new scientific possibilities; dreams of studying genomics for malaria and other important pathogens now seem more achievable and closer to becoming reality.”

What was learned about anti-malarial resistance in Ghana?
The team showed frontline treatments remain widely effective against local strains in Ghana currently. However, ongoing monitoring is essential, including to protect high-risk groups that receive targeted interventions.
The team did not find evidence of resistance to artemisinins – the current front-line and best treatment for P. falciparum. Partial resistance to artemisinins has been detected in southeast Asia and eastern Africa. Ongoing monitoring for resistance will be essential as the spread of this resistance could be devastating for control efforts.
Although mutations associated with resistance to the antimalarial drugs sulfadoxine and pyrimethamine (SP) were found, the especially dangerous mutations causing ‘high-level’ resistance to SP were not found. This is reassuring, because SP is used for prophylaxis in young children and during pregnancy in Ghana.

New vaccine rollout
The researchers also discovered multiple genetic differences between circulating malaria strains and the csp gene sequence targeted by newly recommended malaria vaccines. This was possible by sequencing longer DNA molecules, an advantage of using nanopore technology.
While requiring further study, these have the potential to impact the latest vaccine rollouts across Africa. But by using this new rapid, accurate and affordable genomic surveillance technique, countries deploying these new vaccines over the coming years will be able to detect and monitor changes in the csp gene.
‘Decentralisation and democratisation’
“A key motivation was to drive the decentralisation and democratisation of genomics,” says Dr William Hamilton from the Genomic Surveillance Unit at the Wellcome Sanger Institute.
“The repeated evolution and spread of resistance to key antimalarial drugs has thwarted efforts to eliminate malaria over the last 70 years. The expansion of molecular surveillance capacity in Africa is critical, to monitor emerging drug and diagnostic test resistance, and for the deployment of new malaria vaccines.”
Dr Lucas Amenga-Etego, from the West African Centre for Cell Biology of Infectious Pathogens (WACCBIP), agrees. “There remains a need for upscaling sequencing capacity development in malaria-endemic countries to bridge the Global North and South sequencing divide – including bioinformatics and data analytics infrastructure. This should be a key goal for the global pathogen genomics community going forward.”

Read the full paper: S.T. Girgis et al. (2023) Drug resistance and vaccine target surveillance of Plasmodium falciparum using nanopore sequencing in Ghana. Nature Microbiology
Also check out more thoughts on this exciting new study from the team responsible in this ‘Behind the Paper’ blog.

